It’s often said that one of Canada’s fundamental challenges is too much space, too few people. This makes organizing health care services in less urban locations difficult, and with our older rural-dwelling adults seeking to age in place, providing home and community care services to support them will be a hurdle overcome by particularly creative policy solutions.
However, Canada isn’t the only place in the world with an ageing population that wants community-based supports to enable ageing in place. I recently spoke at the Global Conference on Integrated Care in another country that is facing similar challenges and is perhaps Canada’s geographical antithesis: Singapore, a compact, island city-state.
Despite its density, Singapore has many similarities to Canada, and Toronto in particular, such as high life expectancy of 82 years and a rapidly ageing population. Of the approximately 5.7 million Singaporeans, comprised mainly of those of either Chinese, Indian or Malay descent, 14% are aged 65 and over, however, by 2030 25% of the population will be 65 and over. With Singapore ageing faster than many other countries, including Canada, its focus is quickly turning on how to best meet the needs of its older adults. Furthermore, Singapore and Canada’s health care systems still rely heavily on hospital and institutional-based care, despite older adults in both countries overwhelmingly stating their desire to age at home and in the community.
To satisfy the preferences of its older adults, Singapore, like Canada, has begun to reorganize its health care system to improve accessibility, affordability and quality – with a new approach which is expected to be rolled out by 2020. One aspect of the plan is Singapore’s adoption of three regional health systems, which are intended to truly integrate care across different settings using a population health approach.
Even with the effort to reorganize health care delivery, many community-dwelling older adults in Singapore continue to face health and social challenges that can be further characterized by their ethnicity as well. For example, in Singapore, amongst the three broad ethnic groups that make up the population, Chinese Singaporeans are at the lowest risk of falling, while Indians are at the highest risk, followed by Malays. Indians and Malays have also been found to experience a higher prevalence of depressive symptoms and disability. The range of risk for falls and other issues amongst these different groups also reflect disparities in socioeconomic status, use of health services, the prevalence of cognitive issues and cultural specific issues as well.
The cultural differences among Singapore’s population go beyond influencing health risks to also affecting the community life of older adults. For example, Indian and Malay are more likely to socialize their children, and in turn be socialized themselves, through religious, cultural and family events, than Chinese Singaporeans are. For policy makers and organizations in Singapore, this means in order for social programs for older adults to be inclusive of and meaningful to Indians and Malays, they may need to be more encompassing of cultural and religious themes and activities.
The biggest threat for both Canada and Singapore, however, to advancing the development of home and community care is addressing the critical and growing shortages of health care professionals, principally nurses and personal support workers, that will be crucial to enabling more older adults to age and receive care in their own homes and communities. The inability to develop enough capacity in our respective home and community care sectors has otherwise made it hard to move and keep people out of more costly hospitals and community settings. Often in both countries, the reality is that the gaps in our care systems end up being borne by family caregivers. A recent survey showed that 40% of caregivers in Singapore have at least one caregiving-related need which helps to explain the significant emotional stress experienced by both caregivers and those they support when unmet needs exist.
Our common challenges have allowed us to realize a great opportunity towards working more closely together to learn from each other as we address mutual areas of interest.
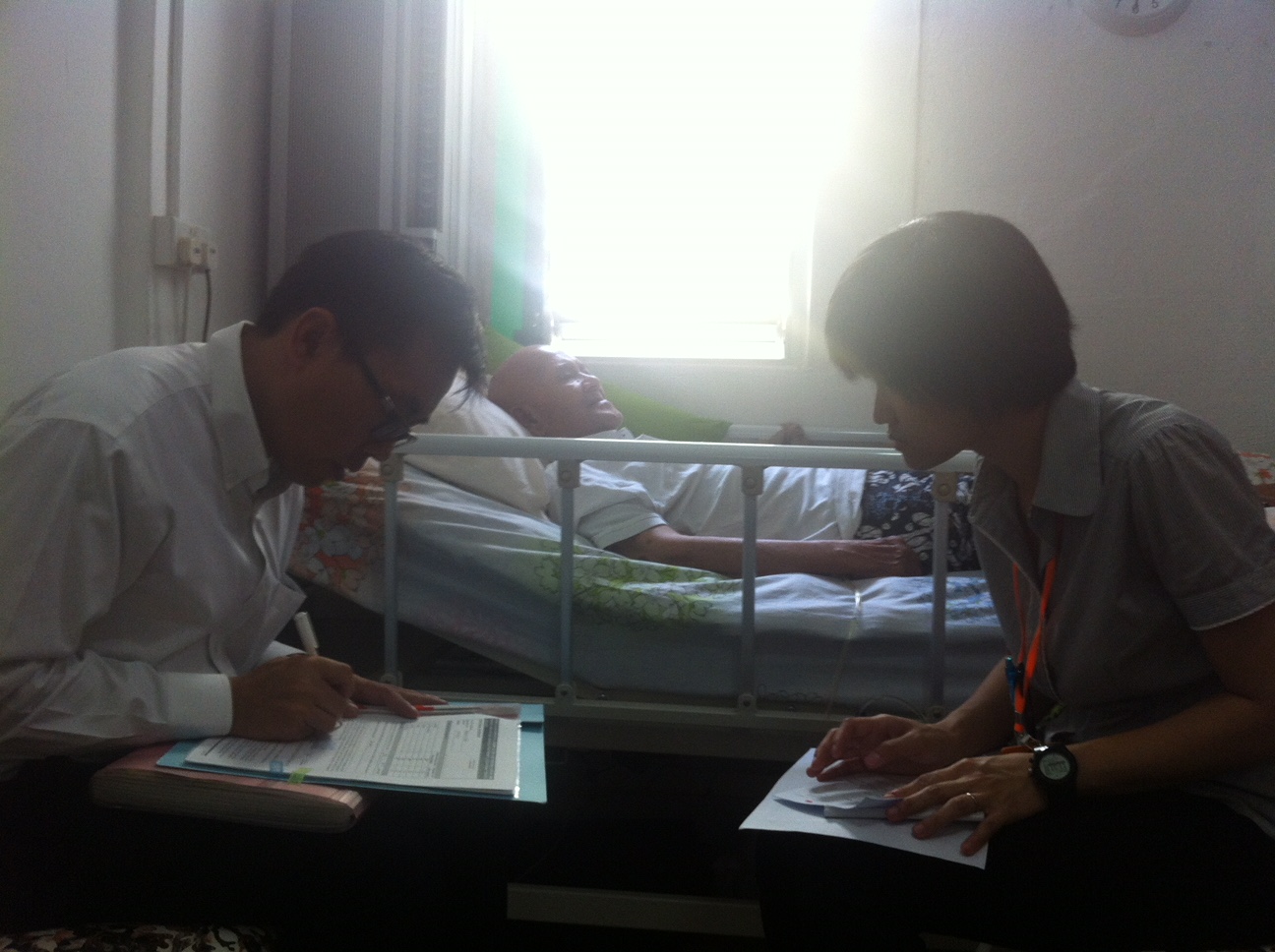
In 2015, I was first invited to Singapore through the TSAO Foundation’s Expert Series Program where I was able to share Sinai Health System’s emerging Population Health Approach along with our innovative Acute Care for Elders (ACE) Strategy and our Government of Ontario’s Seniors Strategy. In 2016, Sinai Health System and the Government of Ontario hosted a delegation from Singapore so we could continue exchanging strategies and ideas. Now, a healthy knowledge exchange is well underway with Sinai Health System’s Healthy Ageing and Geriatrics Program increasingly hosting learners and observers in geriatric medicine and health care administration from Singapore as well.
The Asian tiger is ageing fast but so are our polar bears. Indeed, while there is more than geography and distance that separates Canada and Singapore, the two countries share a similar pressing need to reorganize health care delivery to enable and support an ageing population to remain independently at home. We look forward to achieving more by working together in our collective efforts over the coming decade.
Date modified: 2018-02-22

