Every year thousands of Canadians enter medical school and start a journey where they meet, learn from and work with many talented medical professionals including: pediatricians, family physicians, general internists, emergency medicine physicians, surgeons, obstetricians, gynecologists, anesthesiologists, psychiatrists and many others. However, medical students are rarely given the opportunity to engage with geriatricians during their medical education. In fact, many medical trainees may go through their entire medical education without ever being taught about the unique health needs that older people may have.
This gap in medical training has very real and growing health care consequences for our ageing population. Our older population – those aged 65 or over – is expected to double in the coming decades and we will need many more care providers with specialized skills and expertise to support older adults to remain as healthy as possible as they age. There are currently only 248 geriatricians in Canada. That’s one for every 20,914 older Canadians. It’s estimated that we need at least 500 geriatricians to care for today’s older patients. Some provinces and territories have zero or one geriatrician to support their ageing populations.
In order to achieve our collective health human resource goals and needs, medical schools will need to be at the front lines of preparing medical trainees to provide care for older patients, who they are most likely to meet as doctors.
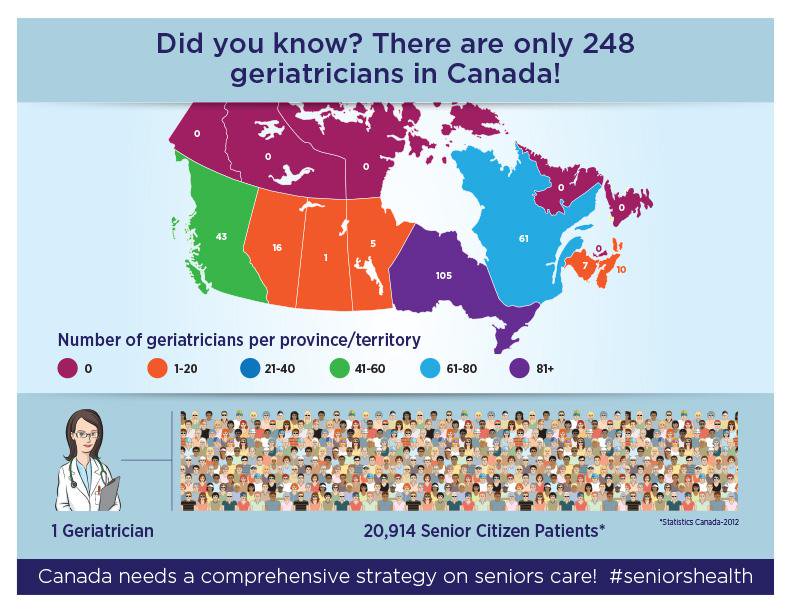
Image courtesy of the Canadian Medical Association.
Medical schools today aren’t thoroughly preparing their students to provide appropriate care to these patients. So, what are they exposing their students to?
Even a cursory look at medical school curricula would reveal the disparity between the emphasis placed on geriatrics and that placed on, say, pediatrics. Undergraduate medical students receive about 82 hours of training in geriatrics on average. There are only six medical training programs that require a rotation in geriatrics, while a pediatrics rotation is mandatory everywhere. However, medical students today are much more likely to provide care for older patients than younger patients in their careers, especially now that there are more Canadians over 65 than those who are under 15.
Even with our rapidly ageing population, there remain naysayers who contest the idea that we need more geriatricians. Older adults, they say, have many of the same issues of younger patients. The thought is that the only difference is that older patients may just have more conditions. This argument is overly simplistic, however, as mounting research has now shown us that as people age their bodies react differently to therapies, which are usually only tested in younger people. With the added challenges of dementia, functional and social challenges that many older adults can often face as they age, primary care providers who are and will be leading the provision of geriatric care in Canada need to be equipped to work effectively and efficiently with this growing population, while also being able to access the right geriatric expertise to support them and their patients when needed.
So, we’re faced with the reality of an ageing population that will benefit from the support of more geriatricians and medical schools that continue to emphasize the needs of younger patients.
As leaders in geriatrics and healthy ageing, we invest heavily in encouraging and training the next generation of specialists and health care providers who will deliver care to older patients in the future. We take pride in training learners in geriatric medicine, psychiatry, rehabilitation and emergency medicine from around the world through our structured clinical training programs. Last year alone, we hosted 205 interprofessional learners in geriatric medicine, including nurses, social workers, pharmacists and many others at all levels from medical students to residents and fellows. Overall, since we launched our Healthy Ageing and Geriatrics Program, more than 750 learners have come to train with us from all around the world including from countries beyond North America such as Spain, Ireland, the United Kingdom, Egypt, Hong Kong, Brazil, Israel, Pakistan, Singapore, the United Arab Emirates and the Caribbean.
To further address the growing health human resources gap, in 2012 we established the Savlov/Schmidt Summer Scholars Program. The program provides unique and structured learning opportunities for students to gain valuable research or project experience in a health care setting and to encourage them to consider a future career in the fields of ageing and geriatrics.
The program matches a staff geriatrician or another health care professional with an undergraduate university or medical or other health care professional student to work on a research project together. The students also benefit from getting further opportunities to shadow geriatricians and other clinical team members in a variety of settings to develop a greater understanding of the many ways through which geriatric care can be provided.
The program further offers opportunities for staff in our programs to provide research or project experiences and mentorship for students from a variety of disciplines in an effective and organized manner. The program also aims to meet the needs of interested students who are eager to gain valuable research experience as well. This year’s Savlov/Schmidt Summer Scholars – Stephanie Brooks, Adrian Chan, Victoria Chuen, Shionne Hitchman and Aliya Nowaczynski – conducted research on a range of topics including natural disaster preparedness strategies for older adults, documenting delirium in discharge summaries, supporting gerontology training among social workers, geriatrics education for orthopedic surgery residents, and fostering professionalism among medical students. We are proud that the students that we have hosted through this program tell us each and every year how much they have learned and come to appreciate what a career in geriatrics could hold for them.
Ensuring that students and residents are exposed to the principles and practices of providing care to older adults is a first step towards meeting the health and social care needs of older adults. While our efforts aren’t designed to create geriatricians – we are glad we are helping future care providers to gain an appreciation for caring for older adults and possibly choose careers in geriatrics. Of course, we will not rest either until we ensure that geriatrics education becomes integrated in every medical, nursing, pharmacy, therapy and social work school’s curriculum.
Date modified: 2017-08-18

